The Cellular Architecture of Immunity: A Systems Overview of Human Immune Cell Types and Their Functional Networks
Mapping the Interconnected Roles of Immune Cells in Defense, Surveillance, and Homeostasis
Immune Cell Interconnectivity in Biotechnology and Medicine
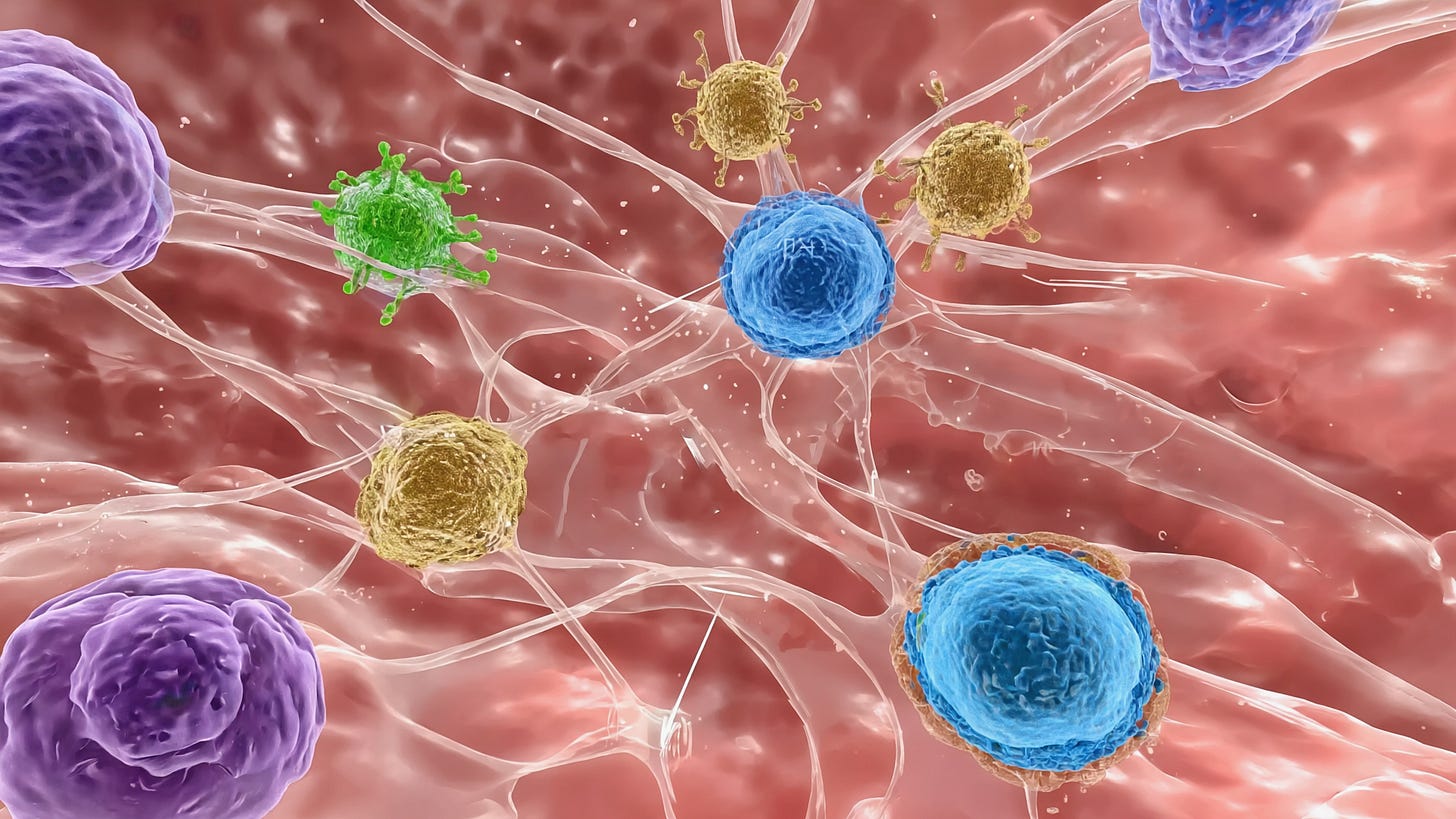
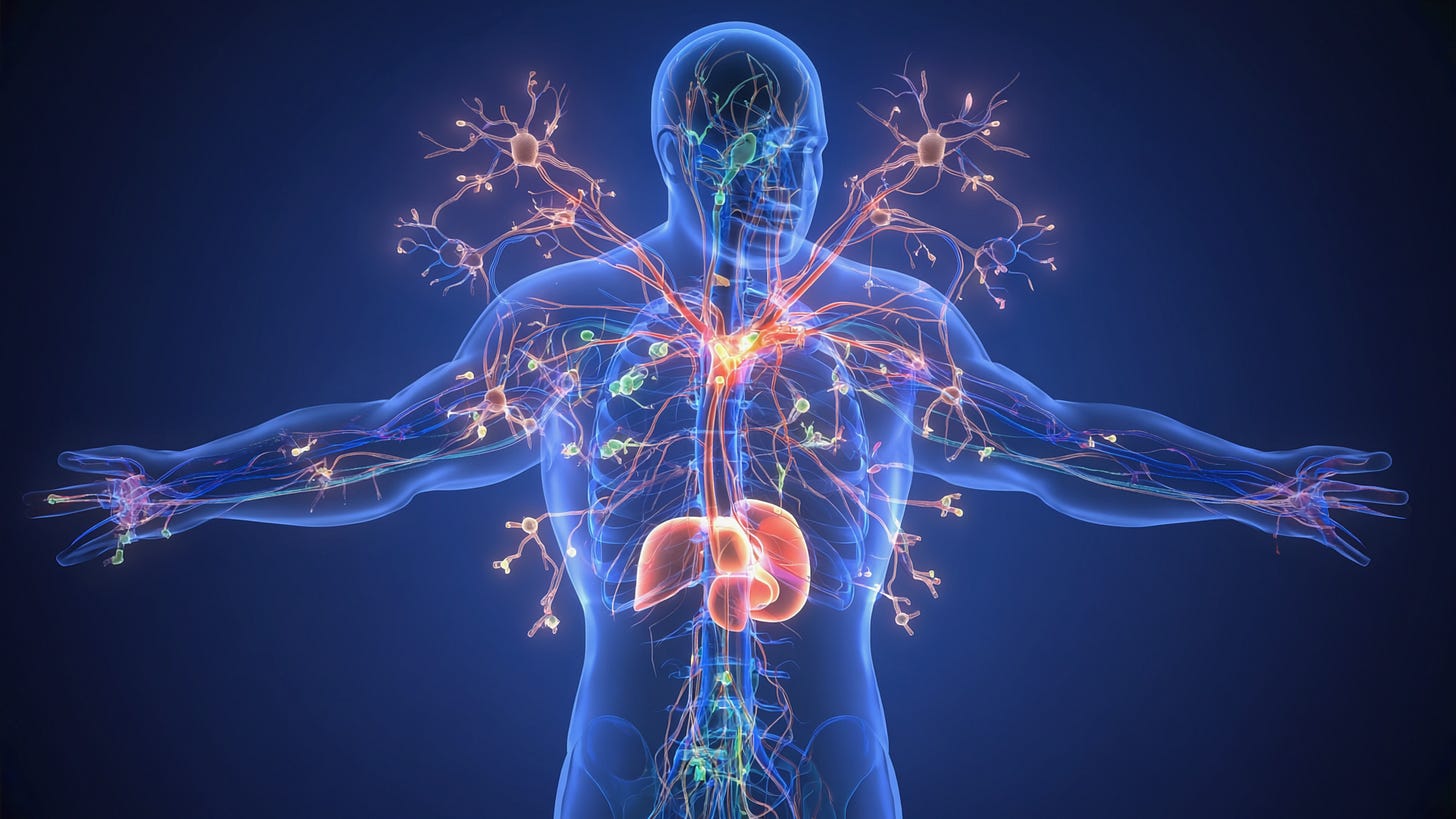
A central tenet of modern immunology is that immune cells do not operate in isolation; rather, their function is emergent arising from reciprocal, context-dependent interactions across multiple lineages. The immune system comprises a diverse array of cell types, each with distinct phenotypic markers, effector functions, tissue localization patterns, and differentiation trajectories. These cells form a densely interconnected communication network mediated by cytokines, chemokines, cell surface receptors, antigen presentation, and metabolic cues.
Understanding this network is critical in biotechnology and medicine because immune dysregulation is not typically the result of a single cellular defect, but rather a breakdown in the regulatory balance between immune subsets. This systems-level dysfunction underlies the pathogenesis of cancer, autoimmunity, chronic inflammation, and vaccine non-responsiveness and provides numerous leverage points for therapeutic intervention.
Innate Immune Cells: The First Responders and Orchestrators
Neutrophils are polymorphonuclear granulocytes that rapidly migrate to sites of infection or injury, where they release reactive oxygen species (ROS), proteases, and form neutrophil extracellular traps (NETs). Though short-lived, they are crucial for initial microbial clearance and modulate adaptive responses via cytokine release and antigen processing.
Monocytes circulate in the blood and differentiate into macrophages or inflammatory dendritic cells in tissues. Macrophages exhibit remarkable plasticity, shifting between pro-inflammatory (M1) and tissue-repair (M2) phenotypes. They phagocytose pathogens, clear apoptotic cells, and present antigen via MHC II to CD4+ T cells.
Dendritic cells (DCs) are professional antigen-presenting cells (APCs) with specialized pattern recognition receptors (PRRs). Upon pathogen recognition, they mature, migrate to lymph nodes, and initiate adaptive immunity by activating naïve T cells.
Mast cells and basophils, loaded with preformed granules of histamine and cytokines, are key mediators of allergic reactions and parasite defense. Mast cells, especially, reside in tissues and act as immune sentinels.
Eosinophils are effector cells in type 2 immunity (anti-parasitic, allergic responses) and contribute to tissue remodeling and inflammation through degranulation.
Natural Killer (NK) cells are cytotoxic lymphocytes of the innate lineage that recognize stressed or infected cells through a balance of activating and inhibitory receptors, including those sensing MHC class I downregulation. NK cells kill target cells via perforin/granzyme release and contribute to antibody-dependent cellular cytotoxicity (ADCC) via CD16.
Innate Lymphoid Cells (ILCs) are tissue-resident lymphocytes that mirror T helper subsets in cytokine production (ILC1/Th1, ILC2/Th2, ILC3/Th17-like). They shape local immunity, epithelial repair, and microbiome balance.
Adaptive Immune Cells: Specificity and Memory
CD4+ T helper (Th) cells differentiate into functional subsets Th1, Th2, Th17, Tfh, and Treg based on cytokine milieu and antigen presentation context. They direct immune responses by secreting cytokines and engaging with B cells, macrophages, and other T cells.
CD8+ cytotoxic T lymphocytes (CTLs) recognize antigenic peptides presented by MHC I on infected or malignant cells and eliminate them through perforin and granzyme-mediated apoptosis. Their function is critical in antiviral and anti-tumor immunity.
Regulatory T cells (Tregs) expressing FOXP3 suppress excessive immune activation and maintain tolerance by releasing IL-10 and TGF-β, and through contact-dependent mechanisms involving CTLA-4 and LAG-3.
B cells, upon encountering antigen and T cell help, differentiate into plasma cells (antibody-secreting) or memory B cells. Their antibodies neutralize pathogens, opsonize targets, and activate complement.
Follicular helper T cells (Tfh) specialize in helping B cells within germinal centers, supporting somatic hypermutation and class switch recombination.
Gamma-delta (γδ) T cells and NKT cells are unconventional lymphocytes with rapid, innate-like responses to stress antigens and glycolipids presented via CD1d.
Functional Integration: From Defense to Dysregulation
Each immune cell subtype contributes to a stage of the immune response, but their effectiveness depends on dynamic cooperation:
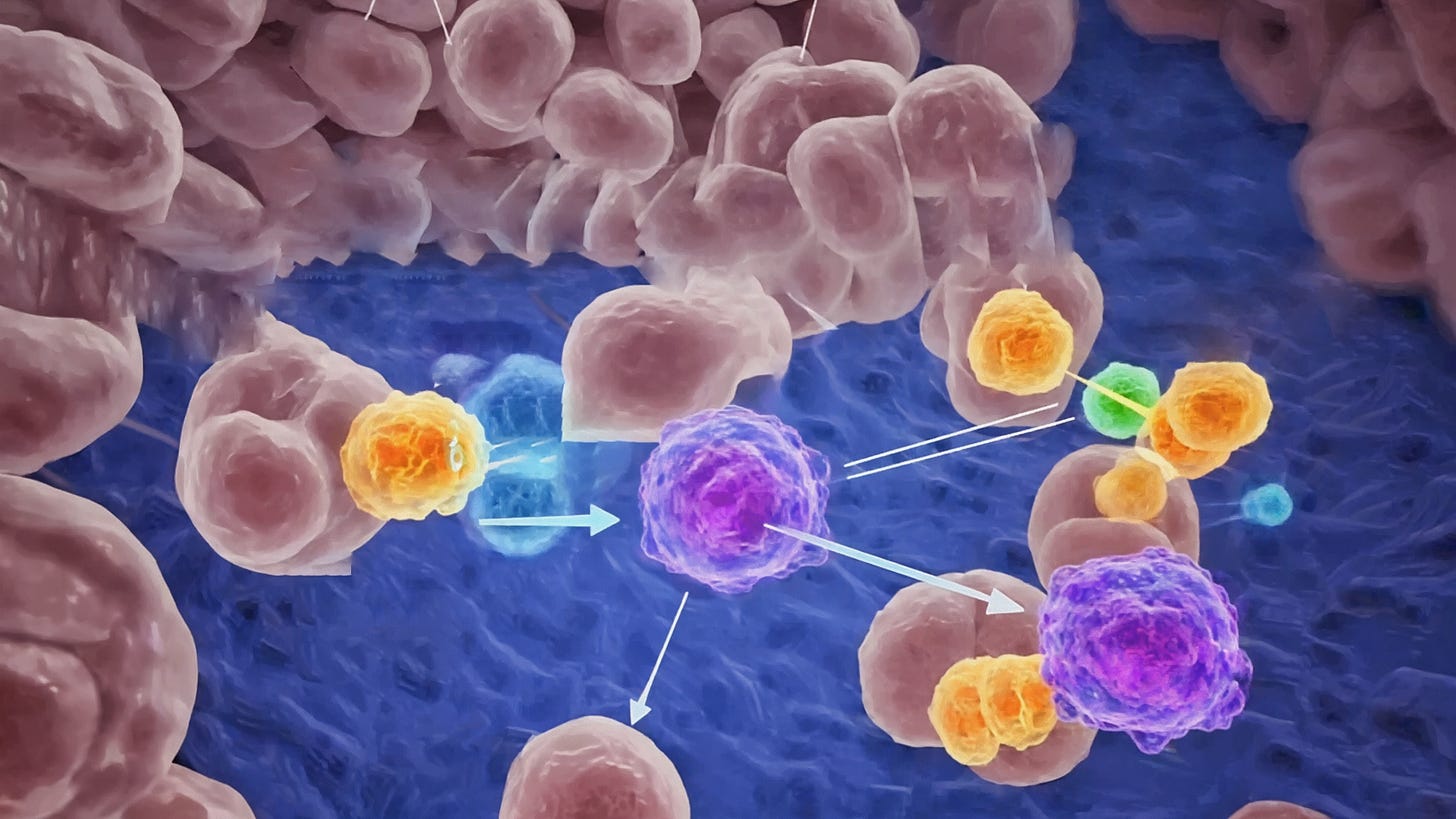
During vaccination, dendritic cells prime naïve CD4+ and CD8+ T cells, which then orchestrate antibody generation by B cells, supported by Tfh cells. ILCs at the injection site modulate early inflammation and tissue signaling.
In cancer immunotherapy, checkpoint blockade (e.g., anti-PD-1, anti-CTLA-4) seeks to reactivate exhausted CD8+ T cells, but outcomes depend on the presence of tumor-infiltrating DCs, Tregs, MDSCs, and local macrophage polarization.
Autoimmune disease often results from a failure of Tregs to suppress autoreactive Th17 or Th1 cells, inappropriate antigen presentation by DCs, and B cell autoantibody production. Therapeutics that restore regulatory balance like low-dose IL-2 or B cell depletion require precise systems understanding.
In chronic infections (e.g., HIV, HCV), prolonged antigen exposure leads to T cell exhaustion, DC dysfunction, and altered NK cell and monocyte phenotypes hallmarks of immunoparalysis.
Why This Matters for Biotech and Therapeutic Innovation
Biotechnological advances increasingly rely on the ability to harness or modulate immune system complexity:
CAR-T cell therapies engineer CD8+ T cells to recognize tumor antigens, but success depends on overcoming immunosuppressive macrophage and Treg networks.
mRNA vaccine design requires antigen optimization for DC uptake, MHC presentation, and Tfh/B cell stimulation, alongside ILC2- or ILC3-driven mucosal responses in some platforms.
Bispecific antibodies are designed to tether T cells or NK cells to tumor targets, requiring understanding of Fc receptor interactions and immune synapse dynamics.
Microbiome-immune interactions increasingly show that ILCs, macrophages, and Th17 cells are modulated by gut flora, making immune profiling essential for gut-targeted therapeutics.
Immunology has entered a systems era where successful therapeutic strategies depend not just on modulating one cell type, but on reprogramming immune networks as a whole. A detailed, structured understanding of immune cell crosstalk is no longer optional, it is a prerequisite for innovation.
Hematopoiesis: The Root of All Immune Lineages
The immune system’s extraordinary cellular diversity originates from a single biological process: hematopoiesis. This highly regulated mechanism is responsible for the continuous production, differentiation, and maturation of all blood and immune cells from multipotent progenitor cells, known as hematopoietic stem cells (HSCs).
Overview of Hematopoietic Stem Cells (HSCs)
HSCs are rare, self-renewing, multipotent cells that reside primarily within the specialized niches of bone marrow. These niches provide essential microenvironmental cues, such as cell adhesion signals, cytokines (e.g., stem cell factor [SCF], interleukin-3 [IL-3], thrombopoietin [TPO]), chemokines (e.g., CXCL12), and extracellular matrix interactions—that tightly regulate stem cell quiescence, self-renewal, differentiation, and mobilization. Phenotypically, human HSCs are typically identified by the expression of surface markers including CD34+, CD38–, CD90 (Thy-1)+, and CD45RA–.
Functionally, HSCs can differentiate into two main lineages, termed the myeloid and lymphoid lineages, through a series of defined intermediate progenitor stages, each marked by distinct cell-surface receptors and transcriptional programs. Their exceptional regenerative capacity is vital, as billions of blood cells, including immune effector cells, must be replenished daily.
Myeloid vs. Lymphoid Lineage Differentiation
Differentiation from HSCs begins with their asymmetric division into multipotent progenitors (MPPs). Early lineage fate determination occurs downstream of MPPs, resulting in two primary lineage branches:
Myeloid lineage: The common myeloid progenitor (CMP) gives rise to a wide variety of innate immune cells, including:
Monocytes and macrophages: involved in pathogen phagocytosis, inflammation, and antigen presentation.
Dendritic cells: antigen-presenting cells bridging innate and adaptive immunity.
Granulocytes: neutrophils, eosinophils, and basophils, key effectors in early infection responses, inflammation, allergy, and antiparasitic defenses.
Mast cells: tissue-resident cells critical in allergy and tissue remodeling.
Additionally, CMPs give rise to erythroid (red blood cells) and megakaryocyte (platelets) lineages, essential for oxygen transport and blood clotting.
Lymphoid lineage: Common lymphoid progenitors (CLPs) generate cells central to adaptive immunity, including:
B lymphocytes (B cells): antibody-producing cells central to humoral immunity.
T lymphocytes (T cells): mature in the thymus to become helper (CD4+), cytotoxic (CD8+), or regulatory (Treg) cells essential in adaptive immunity and tolerance.
Natural killer (NK) cells: innate-like lymphocytes critical for early defense against virally infected and tumor cells.
Innate lymphoid cells (ILCs): specialized lymphoid populations involved in tissue homeostasis and mucosal immunity.
Transcription factors such as PU.1, CEBPA, RUNX1, GATA-1, Ikaros, E2A, and PAX5 orchestrate myeloid versus lymphoid lineage commitment. Cytokine signaling (e.g., IL-7 for lymphoid lineages, GM-CSF for myeloid lineages) further refines these fate decisions.
Role of Bone Marrow and Thymus
Bone marrow is the primary site of hematopoiesis and provides a highly structured niche for HSC maintenance, self-renewal, and differentiation. Within marrow cavities, a specialized microenvironment is maintained by stromal cells, osteoblasts, endothelial cells, and mesenchymal stem cells. Bone marrow also hosts the developmental maturation of B cells through sequential rearrangement of immunoglobulin gene loci, culminating in immature B cells exiting to secondary lymphoid organs.
The thymus, a specialized primary lymphoid organ located in the anterior mediastinum, is essential for T cell development. Immature lymphoid progenitors migrate from the bone marrow to the thymus, where they undergo complex developmental checkpoints:
Positive selection ensures T cells recognize self-MHC molecules.
Negative selection eliminates strongly autoreactive T cells, preventing autoimmunity.
Surviving thymocytes mature into naïve CD4+ helper, CD8+ cytotoxic, or regulatory T cells, exiting the thymus to seed peripheral lymphoid organs and tissues.
Both organs are subject to age-associated changes—thymic involution and shifts in bone marrow niche composition—contributing to diminished immune function (immunosenescence) in elderly populations.
Integrating Lineage Differentiation and Immune Functionality
Understanding hematopoietic lineage differentiation is pivotal for biotechnology and clinical medicine, informing approaches like:
Bone marrow transplantation: restoration of hematopoiesis in malignancies (e.g., leukemia) or autoimmune diseases.
Gene therapy: correction of genetic disorders (e.g., SCID, X-linked immunodeficiency).
Immunotherapy: ex vivo expansion or engineering of specific immune subsets (CAR-T cells, engineered dendritic cells).
Stem cell mobilization: strategies leveraging HSC migration pathways to harvest cells for transplantation or gene editing.
Moreover, dysregulated lineage differentiation pathways underpin numerous pathological states, from leukemias (aberrant progenitor differentiation) to autoimmune disorders (imbalance between effector and regulatory lymphocyte subsets). The framework of hematopoiesis and immune lineage differentiation underpins the entirety of immune functionality, informing both our fundamental understanding and practical manipulation of immune responses.
Innate Immune Cells: The First Line of Defense and Immune Sentinels
Innate immune cells form the critical first barrier against pathogens, tissue damage, and malignancies. They respond swiftly, leveraging evolutionarily conserved pattern recognition receptors (PRRs) to sense pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs). This initiates immediate defense mechanisms and inflammatory cascades, shaping subsequent adaptive immune responses through complex cellular interactions and cytokine signaling networks.
Cellular Components and Their Functional Specializations
a. Monocytes & Macrophages
Monocytes (~10–15 µm in diameter) originate in the bone marrow, circulate briefly in blood, and rapidly infiltrate tissues during inflammation. Upon tissue entry, monocytes differentiate into macrophages, which demonstrate substantial morphological plasticity and polarization capacity:
M1 Macrophages (classically activated): Induced by IFN-γ, TNF-α, or microbial stimuli (LPS); characterized by pro-inflammatory cytokine secretion (IL-1β, IL-6, TNF-α), high phagocytic capacity, robust ROS and nitric oxide (NO) production, and promotion of Th1 responses.
M2 Macrophages (alternatively activated): Induced by IL-4, IL-13, or TGF-β; involved in resolution of inflammation, tissue remodeling, fibrosis, and regulatory activities, secreting IL-10 and TGF-β.
Specialized tissue-resident macrophages include:
Microglia (CNS): Maintain neural homeostasis, synaptic pruning, modulate neuroinflammation.
Kupffer Cells (liver): Clear blood-borne pathogens, apoptotic cells, endotoxins; modulate hepatic immunity.
Alveolar Macrophages (lung): Surfactant homeostasis, pathogen clearance, regulation of pulmonary inflammation.
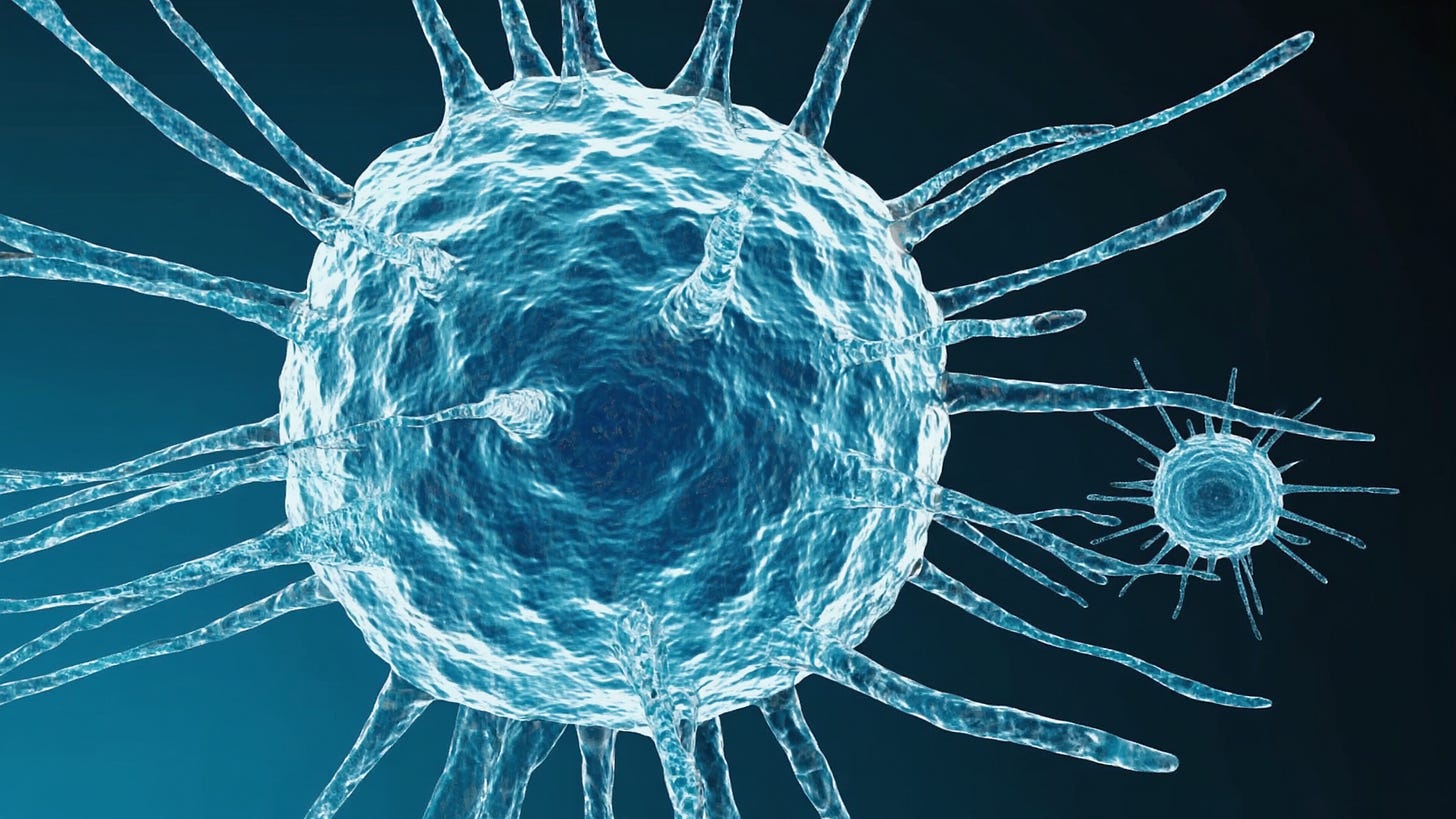
b. Dendritic Cells (DCs)
Dendritic cells (10–20 µm) represent the primary interface linking innate and adaptive immunity. They continuously surveil tissues via long membrane protrusions, sampling antigens through macropinocytosis, receptor-mediated endocytosis, and phagocytosis. DC maturation, triggered by PAMP recognition (via TLRs, NOD-like receptors [NLRs], or RIG-I-like receptors [RLRs]), induces enhanced expression of MHC molecules and costimulatory molecules (CD80, CD86), migration to draining lymph nodes, and secretion of cytokines (IL-12, IL-23, IL-10).
Major DC subsets:
Classical DC1 (cDC1): Specialized for cross-presentation to CD8+ T cells, critical for antiviral and antitumor responses.
Classical DC2 (cDC2): Activate CD4+ T cells, support Th2 and Th17 differentiation.
Plasmacytoid DCs (pDCs): Potent producers of type-I interferons (IFN-α, IFN-β), essential in antiviral defense.
c. Neutrophils
Neutrophils (12–15 µm), representing ~60–70% of circulating leukocytes, rapidly infiltrate infection sites guided by chemotactic factors (IL-8, C5a, LTB4). They contain cytoplasmic granules (primary azurophilic: myeloperoxidase, elastase; secondary specific: lactoferrin, lysozyme), enabling immediate pathogen killing via:
Phagocytosis and ROS Production: NADPH oxidase generates ROS within phagosomes, effectively killing pathogens.
Degranulation: Extracellular release of antimicrobial factors.
NETosis: Formation of neutrophil extracellular traps (NETs)—chromatin webs embedded with antimicrobial proteins (e.g., histones, elastase)—capturing and killing extracellular pathogens.
d. Eosinophils & Basophils
Eosinophils (~12–17 µm) possess bilobed nuclei and prominent eosinophilic granules containing major basic protein (MBP), eosinophil cationic protein (ECP), eosinophil-derived neurotoxin (EDN), and eosinophil peroxidase (EPO). Eosinophils mediate responses against parasites (helminths) through cytotoxic granule release and modulate allergic inflammation via IL-4, IL-5, and IL-13 production.
Basophils (~10–14 µm) are rare, granulated cells expressing high-affinity IgE receptors (FcεRI). Activation triggers rapid histamine, leukotriene, and cytokine release, amplifying type-2 immune responses and hypersensitivity reactions.
e. Mast Cells
Mast cells (10–15 µm), strategically positioned at mucosal surfaces and connective tissues, exhibit abundant granules containing histamine, proteases (tryptase, chymase), and cytokines. IgE-FcεRI crosslinking prompts rapid degranulation, driving vasodilation, vascular permeability, bronchoconstriction, and immediate-type hypersensitivity reactions. Mast cells also regulate tissue remodeling, fibrosis, wound healing, and pathogen clearance via innate recognition mechanisms (TLRs, complement receptors).
f. Natural Killer (NK) Cells
NK cells (~12–16 µm), large granular lymphocytes, provide immediate cytotoxic surveillance through recognition of infected, stressed, or transformed cells, integrating signals from activating receptors (e.g., NKG2D, NKp46) and inhibitory receptors (KIRs, NKG2A):
Cytotoxic Effector Function: Release cytotoxic granules containing perforin and granzymes, inducing apoptosis.
Missing-self Recognition: Detect abnormal MHC class I expression, characteristic of tumor or virally infected cells.
Antibody-dependent Cellular Cytotoxicity (ADCC): Eliminate antibody-coated targets via CD16 (FcγRIII).
NK cells also modulate adaptive responses through IFN-γ secretion, enhancing Th1 polarization and dendritic cell maturation.
g. Innate Lymphoid Cells (ILCs)
ILCs (~10–15 µm) represent non-antigen-specific, tissue-resident lymphocytes that rapidly respond to cytokine signals, mirroring T helper subsets functionally:
ILC1 (analogous to Th1 cells): Produce IFN-γ; protect against intracellular pathogens (viruses, bacteria); support macrophage activation.
ILC2 (analogous to Th2 cells): Secrete IL-5, IL-9, IL-13; mediate parasite clearance, allergic inflammation, tissue repair, epithelial barrier integrity.
ILC3 (analogous to Th17 cells): Produce IL-17, IL-22; critical in mucosal immunity, antifungal responses, microbiota-immune crosstalk.
ILCs rapidly orchestrate immune responses, particularly in mucosal tissues, influencing local inflammation, repair, and homeostasis.
Clinical and Biotechnological Implications
Dysregulated innate immunity underlies numerous pathologies, including chronic inflammation, autoimmunity, cancer progression, and infectious disease susceptibility. Therapeutically targeting innate immune cells—via macrophage polarization modulators, dendritic cell-based cancer vaccines, NK-cell adoptive therapy, or blockade of mast cell-mediated allergy—represents emerging frontiers in immunotherapy and precision medicine.
Innate immune cells form a sophisticated frontline network, dynamically sensing and responding to diverse threats, thus fundamentally shaping broader immune system function and therapeutic intervention strategies.
Adaptive Immune Cells: Precision, Diversity, and Immune Memory
Adaptive immunity is characterized by remarkable antigenic specificity, receptor diversity, clonal expansion, and memory formation. It comprises specialized lymphocytes—B cells and T cells—which undergo complex developmental programs to generate antigen-specific responses with high precision and enduring immunological memory.
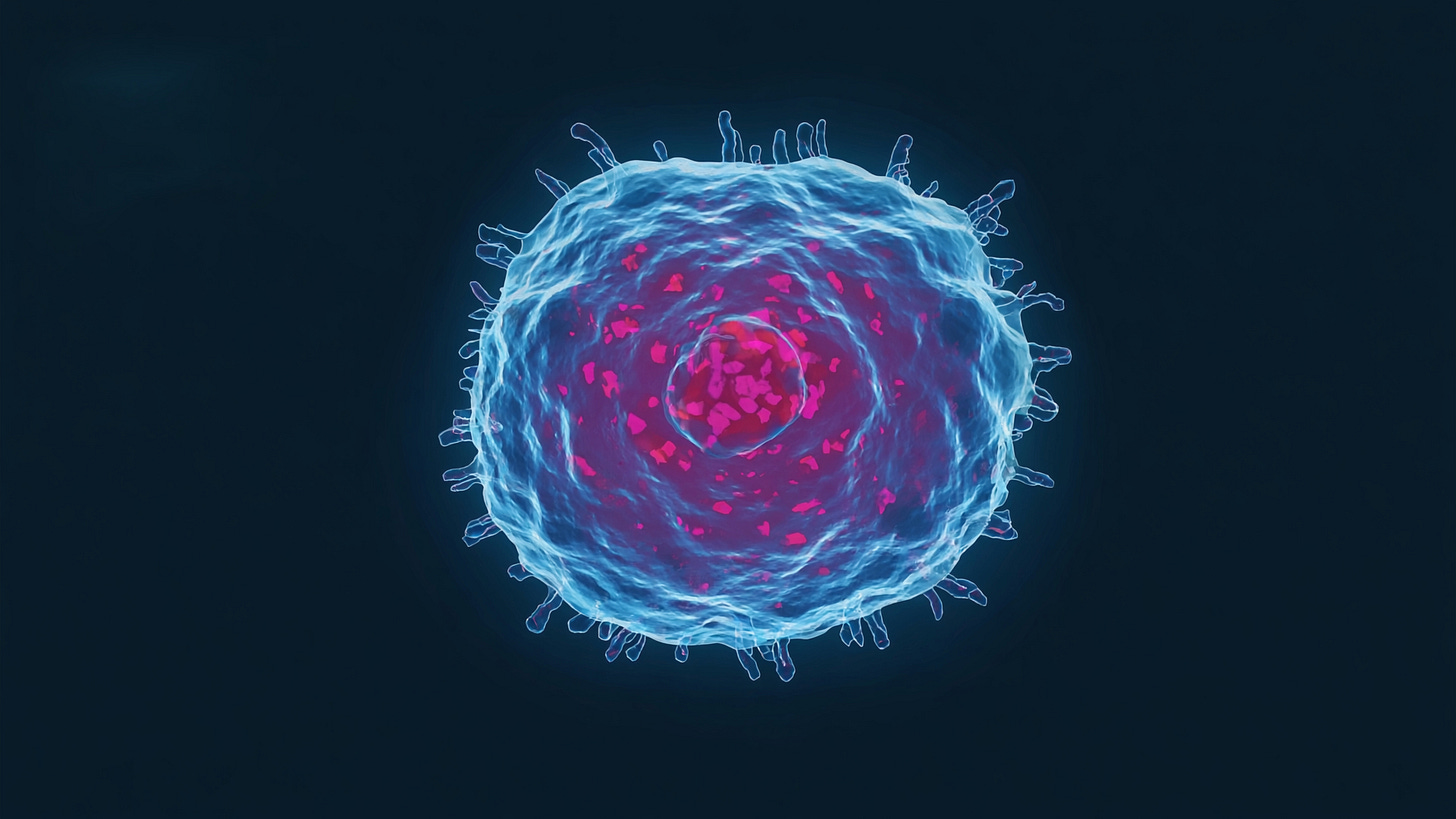
a. B Cells: Architects of Humoral Immunity
B lymphocytes (B cells) mediate humoral immunity through antibody production. Originating from hematopoietic progenitors in the bone marrow, they express clonally unique B cell receptors (BCRs), membrane-bound immunoglobulins (IgM and IgD initially), which recognize specific epitopes on pathogens.
B Cell Subsets and Functions
Naive B Cells:
These mature yet antigen-inexperienced cells circulate through secondary lymphoid organs (lymph nodes, spleen, mucosal-associated lymphoid tissues), awaiting antigen encounter. Upon antigen recognition via the BCR, naïve B cells internalize antigenic material, process it, and present peptides on MHC class II molecules, facilitating cognate interaction with T follicular helper cells (Tfh).Plasma Cells:
Following activation and differentiation signals—primarily IL-21 from Tfh cells—activated B cells transform into antibody-secreting plasma cells. Morphologically distinct, plasma cells possess extensive rough endoplasmic reticulum for high-rate antibody synthesis (several thousand Ig molecules per second). Short-lived plasma cells reside transiently in lymphoid organs, whereas long-lived plasma cells home to specialized bone marrow niches, ensuring sustained antibody titers.Memory B Cells:
Generated concurrently during germinal center (GC) reactions, memory B cells persist for years or decades post-exposure. They express class-switched antibodies (IgG, IgA, IgE) with high affinity and rapidly expand upon subsequent antigen re-exposure, enabling accelerated and robust secondary immune responses.
Antibody Production and Class Switching
Antibody diversification and maturation occur within germinal centers of secondary lymphoid follicles, involving two critical processes:
Somatic Hypermutation (SHM):
Mediated by activation-induced cytidine deaminase (AID), SHM introduces point mutations into the variable (V) regions of immunoglobulin genes, incrementally enhancing antigen-binding affinity—known as affinity maturation. High-affinity B cells are selectively expanded due to improved competition for antigen binding and Tfh cell support.Class Switch Recombination (CSR):
AID-driven CSR rearranges constant-region (C_H) genes in the immunoglobulin heavy chain locus. CSR enables switching from IgM to IgG (various subclasses), IgA, or IgE, each having distinct effector functions:IgG: Complement fixation, opsonization, neutralization.
IgA: Mucosal protection and neutralization of pathogens at mucosal surfaces.
IgE: Parasite clearance, allergic inflammation.
b. T Cells: Regulators and Executors of Cellular Immunity
T lymphocytes (T cells) orchestrate cellular immune responses by interacting with antigen-presenting cells (APCs), recognizing peptide antigens presented by major histocompatibility complex (MHC) molecules via the T cell receptor (TCR).
CD4+ Helper T Cells (Th Cells)
CD4+ T cells recognize peptides presented by MHC class II molecules, coordinating adaptive immunity by differentiating into functional subsets depending on cytokine environments:
Th1 Cells:
Driven by IL-12 and IFN-γ signaling; produce IFN-γ, TNF-α, IL-2, promoting cell-mediated immunity against intracellular pathogens, macrophage activation, and CD8+ T cell cytotoxicity.Th2 Cells:
Differentiation mediated by IL-4; secrete IL-4, IL-5, IL-13, directing immunity against helminths, promoting IgE-mediated allergic responses, eosinophilia, and tissue remodeling.Th17 Cells:
Induced by IL-6, IL-23, and TGF-β; secrete IL-17, IL-22, vital for mucosal defenses, neutrophil recruitment, anti-fungal immunity, and linked with autoimmunity and chronic inflammatory conditions.T Follicular Helper (Tfh) Cells:
Specialized to reside in lymphoid follicles; driven by Bcl6 transcription factor expression, produce IL-21, CXCL13, and express CD40 ligand (CD40L) to assist B cells in germinal center formation, antibody affinity maturation, and class-switching.Regulatory T Cells (Treg):
Expressing Foxp3 transcription factor, maintain immune tolerance, limit excessive inflammation, and prevent autoimmunity via secretion of suppressive cytokines (IL-10, TGF-β) and direct inhibitory interactions (CTLA-4).
CD8+ Cytotoxic T Lymphocytes (CTLs)
CD8+ T cells recognize peptide-MHC class I complexes expressed on all nucleated cells, directly killing infected or malignant cells through:
Perforin/Granzyme-mediated Cytotoxicity: Delivery of cytolytic granules containing perforin and granzymes induces apoptosis of target cells.
Fas Ligand (FasL)-mediated apoptosis: Engagement of Fas receptor on target cells triggers programmed cell death.
Cytokine secretion (IFN-γ, TNF-α): Promotes antiviral immunity, inflammation, and macrophage activation.
Gamma-Delta (γδ) T Cells & NKT Cells
These unconventional T cells bridge innate and adaptive immunity:
Gamma-Delta (γδ) T Cells:
Express γδ-TCR recognizing non-peptide antigens (phosphoantigens, lipids) independently of classical MHC presentation. Abundant in mucosal tissues and skin, providing rapid antimicrobial responses, immunoregulation, and tissue repair.Natural Killer T (NKT) Cells:
Characterized by semi-invariant αβ-TCR recognizing glycolipid antigens presented by CD1d. Upon activation, rapidly secrete cytokines (IL-4, IFN-γ), modulating both innate (NK, dendritic cell function) and adaptive (B cell, conventional T cell responses) immunity. Significant roles in tumor surveillance, autoimmune disease modulation, and pathogen defense.
T Cell Receptor Diversity & MHC Interactions
T cell receptor diversity arises through V(D)J recombination mediated by recombination activating genes (RAG1/2). Positive selection in thymic cortex ensures TCR affinity for self-MHC; negative selection in thymic medulla removes autoreactive T cells. MHC polymorphisms (HLA genes) profoundly influence peptide presentation diversity, susceptibility to autoimmune diseases, and transplant rejection.
MHC Class I:
Present peptides (intracellular origin) to CD8+ T cells; ubiquitously expressed, instrumental in antiviral/tumor immunity.MHC Class II:
Expressed by professional APCs (DCs, macrophages, B cells); present exogenous peptides to CD4+ T cells, orchestrating adaptive responses.
Clinical and Biotechnological Implications
Adaptive immune cells underpin vaccine efficacy, autoimmune disease pathology, transplant immunology, and tumor immunotherapy. Therapeutic exploitation includes:
CAR-T Cells: Genetically engineered T cells targeting tumor antigens.
Checkpoint Blockade Immunotherapy: Enhancing anti-tumor immunity by disrupting inhibitory pathways (PD-1/PD-L1, CTLA-4).
Vaccination Strategies: Designed to induce high-affinity antibody responses and durable memory T/B cell formation.
Autoimmune Therapeutics: Treg expansion, cytokine-targeted biologics (anti-IL-17, anti-IL-6).
Adaptive immunity's complexity underscores its pivotal role in maintaining health, disease pathogenesis, and therapeutic opportunities. This profound understanding continues to drive biomedical innovation.
Bridge Between Systems: Integrating Innate and Adaptive Immunity
The immune system's efficacy relies heavily on finely tuned communication networks bridging innate and adaptive components. This integrative interplay ensures rapid initial responses to pathogens, precision targeting by adaptive lymphocytes, and the establishment of long-lasting immunological memory. Central to these interactions are complex processes involving cytokine-mediated communication, chemokine-driven cell trafficking, sophisticated antigen presentation, and dynamic regulatory feedback mechanisms orchestrated predominantly by dendritic cells (DCs) and macrophages.
Molecular Cross-Talk Between Innate and Adaptive Cells: Cytokines, Chemokines, and Antigen Presentation
Innate immune cells serve as first responders, initiating immune cascades through recognition of pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) via pattern recognition receptors (PRRs), including Toll-like receptors (TLRs), NOD-like receptors (NLRs), and RIG-I-like receptors (RLRs). Upon activation, innate cells rapidly secrete cytokines and chemokines, directly modulating adaptive immunity:
Cytokines:
Innate-derived cytokines such as IL-12, IL-23, IL-6, TNF-α, IL-1β, and type I interferons critically shape adaptive lymphocyte fate decisions:IL-12 and IFN-γ: Direct Th1 differentiation, crucial against intracellular pathogens, enhancing macrophage activation and CD8+ cytotoxic responses.
IL-4, IL-25, IL-33: Promote Th2 differentiation, mediating responses against helminths and allergic inflammation.
IL-6, IL-23, and TGF-β: Drive Th17 cell development, essential for anti-fungal immunity, mucosal defense, and associated with autoimmune diseases.
Type I interferons (IFN-α/β): Enhance dendritic cell maturation and cross-priming, potentiating CD8+ T cell cytotoxicity and antiviral defense.
Chemokines:
Chemokines such as CCL19, CCL21, CXCL13, and CXCL8 coordinate lymphocyte and APC trafficking:CCL19/CCL21: Produced by stromal cells and DCs, guiding naïve T cells and mature DCs to lymph nodes.
CXCL13: Secreted by follicular dendritic cells (FDCs), crucial for attracting B cells into follicles, initiating germinal center reactions.
Antigen Presentation:
Antigen presentation by professional APCs bridges innate recognition and adaptive activation:Classical MHC Class II presentation: DCs, macrophages, and B cells present extracellular-derived peptides to CD4+ T cells, facilitating helper T cell differentiation.
Cross-presentation (MHC Class I): Specialized DC subsets (particularly cDC1) uniquely capture exogenous antigens and present them via MHC class I to CD8+ T cells, critical for antiviral and anti-tumor immunity.
Dendritic Cells and Macrophages: Central Decision-Makers
Dendritic cells and macrophages occupy pivotal positions at the interface of innate-adaptive interactions, dictating the magnitude, quality, and type of adaptive immune responses based on signals received from their environment:
Dendritic Cells (DCs):
DCs decode environmental cues through diverse PRRs and integrate these signals into distinct patterns of costimulatory molecule expression (CD80/CD86, CD40), cytokine secretion, and chemokine receptor expression. Thus, DCs dictate T cell differentiation into distinct effector lineages:DC subsets stimulated by intracellular pathogens (via TLR3, TLR7-9) or type I interferons preferentially induce Th1 and cytotoxic CD8+ responses.
DC subsets activated in mucosal environments (via TLR2, dectin-1) induce Th17 or Th2 responses, directing mucosal immune responses.
DC exposure to regulatory signals (TGF-β, IL-10, retinoic acid) induces tolerogenic DCs, facilitating Treg differentiation, tolerance induction, and immune homeostasis.
Macrophages:
Macrophages interpret local cytokine milieus, dynamically polarizing between inflammatory (M1) and anti-inflammatory/resolution (M2) phenotypes:M1 Macrophages: Activated by IFN-γ, microbial ligands (LPS), or TNF-α; secrete inflammatory mediators (IL-1β, TNF-α, IL-6, IL-12), enhancing adaptive Th1 and Th17 differentiation and potentiate antimicrobial and antitumor responses.
M2 Macrophages: Induced by IL-4, IL-13, IL-10, and TGF-β; secrete anti-inflammatory cytokines, promoting tissue repair, resolution of inflammation, fibrosis, and immune suppression.
These cells act as "immunological rheostats," balancing pathogen clearance with prevention of excessive inflammation and tissue damage.
Feedback Loops Governing Inflammation and Resolution
Immune responses involve intricate feedback loops, precisely modulating inflammation intensity and timing of resolution to maintain tissue homeostasis:
Inflammatory Amplification Loops:
Initial innate recognition rapidly escalates inflammation through cytokine release (IL-1β, IL-6, TNF-α), promoting DC maturation, lymphocyte activation, and further innate cell recruitment. Activated adaptive cells (Th1/Th17) reinforce inflammation through IFN-γ, IL-17, and GM-CSF secretion, establishing positive feedback loops driving acute inflammation.Resolution and Regulatory Feedback Mechanisms:
Concurrently, immune system actively initiates resolution mechanisms to prevent chronic inflammation:IL-10 and TGF-β: Produced by Tregs, macrophages, DCs; dampen antigen presentation, reduce effector cell proliferation, induce regulatory cell phenotypes, and promote tissue repair.
Checkpoint Receptors (CTLA-4, PD-1/PD-L1): Expressed by Tregs and activated T cells; inhibit excessive T cell activation, limit immune-mediated tissue damage, crucially exploited by tumor immune evasion.
Pro-resolving Lipid Mediators (Lipoxins, Resolvins, Protectins): Derived from arachidonic acid and omega-3 fatty acids, these molecules actively terminate neutrophil recruitment, stimulate macrophage polarization towards tissue repair, and orchestrate inflammation resolution and tissue regeneration.
Persistent dysregulation of these loops underpins pathologies including autoimmune diseases, chronic inflammation, allergy, fibrosis, and cancer progression.
Clinical and Therapeutic Implications of Integrating Innate and Adaptive Immunity
The sophisticated interplay between innate and adaptive immunity profoundly influences clinical outcomes and informs therapeutic development:
Cancer Immunotherapy:
Enhancing DC function through vaccines or TLR agonists, manipulating macrophage polarization to disrupt tumor immunosuppression, and checkpoint blockade targeting PD-1/PD-L1 or CTLA-4 to restore adaptive cytotoxicity.Autoimmune and Inflammatory Diseases:
Targeted cytokine blockade (anti-IL-17, anti-IL-6, anti-TNF-α), Treg cell therapy, or modulation of tolerogenic DC populations to restore immune homeostasis.Vaccine Design:
Rational adjuvant incorporation (TLR agonists, STING agonists, or cytokines) to optimally activate DC subsets, modulating adaptive response quality, durability, and specificity.
An advanced understanding of innate-adaptive integration is foundational to immunological homeostasis and therapeutic innovation. Deciphering the complexities of immune cross-talk provides novel insights essential for developing sophisticated immunotherapies and precision-medicine strategies.
Special Topics in Immunology: Advanced Perspectives
In addition to classical immune responses, emerging immunological research has illuminated specialized mechanisms operating in unique tissue microenvironments, shaping immunity and tolerance. These advanced topics—including immune privilege, tissue-resident immune populations, trained innate immunity, and immunosenescence—provide critical insights with significant implications for disease pathology, biotechnology, and therapeutic innovation.
Immune-Privileged Sites: CNS, Eyes, and Testes
Immune privilege characterizes tissues uniquely adapted to limit immune activation, preventing damage from inflammatory responses. Mechanisms include physical barriers, immunoregulatory molecules, and specialized resident immune cells.
Central Nervous System (CNS)
The CNS is isolated by the blood-brain barrier (BBB), composed of specialized endothelial cells connected by tight junction proteins (claudins, occludins) and supported by astrocytes:
Microglia serve as CNS-resident macrophages, originating from yolk-sac progenitors, expressing PRRs (TLR4, TREM2), and conducting continuous immune surveillance.
Astrocytes modulate immune responses via secretion of neurotrophic factors, chemokines, and cytokines (TGF-β, IL-10).
Limited MHC molecule expression and high expression of inhibitory ligands (PD-L1, FasL) prevent unwanted T cell activation.
Disruption of CNS privilege contributes to autoimmune neuroinflammation (e.g., multiple sclerosis) and neurodegenerative diseases (Alzheimer’s, Parkinson’s).
Eyes
Ocular tissues exhibit profound immune privilege, especially in the anterior chamber, cornea, and retina:
Anterior chamber-associated immune deviation (ACAID) prevents systemic delayed-type hypersensitivity via induction of antigen-specific Tregs.
Pigment epithelial cells produce immunosuppressive factors (TGF-β, IL-10, PD-L1), limiting inflammatory responses.
FasL expression by ocular cells actively deletes infiltrating inflammatory T cells.
Loss of ocular privilege results in autoimmune uveitis or inflammatory retinopathies.
Testes
The testes ensure reproductive antigen tolerance through:
Blood-testis barrier (BTB) formed by tight junctions between Sertoli cells, physically segregating developing sperm from systemic circulation.
Sertoli cells express FasL and produce regulatory cytokines (TGF-β, activin A, IL-10) to suppress local immunity.
Disruption causes autoimmune orchitis, impairing fertility.
Tissue-Resident Immune Cells: TRMs, Microglia, Langerhans Cells
Specialized immune populations permanently reside within tissues, integrating immune surveillance with tissue-specific homeostatic functions:
Tissue-Resident Memory T Cells (TRMs)
Persisting within tissues post-infection, TRMs express markers (CD69+, CD103+) and transcription factors (Hobit, Blimp-1):Rapidly produce IFN-γ, TNF-α, IL-17 upon antigen re-exposure.
Provide immediate pathogen containment, especially at mucosal and barrier sites (lung, gut, skin).
Brain Microglia
Resident CNS macrophages, distinct from peripheral macrophages:Continuously survey neuronal synapses, clearing apoptotic cells, myelin debris, pathogens via phagocytosis.
Activated microglia release pro-inflammatory cytokines (IL-1β, TNF-α), neurotoxic mediators (ROS, NO), contributing to neurodegeneration.
Skin Langerhans Cells
Specialized epidermal dendritic cells, expressing langerin (CD207), CD1a, and MHC class II molecules:Efficiently capture and present skin antigens, migrating to lymph nodes upon activation.
Key in initiating tolerance or allergy through induction of Th2/Th17 responses, critical in allergic dermatitis.
Trained Immunity: Epigenetic Memory in Innate Cells
Traditionally, memory responses were attributed solely to adaptive immunity. Recent research reveals innate cells (monocytes, macrophages, NK cells) develop nonspecific memory termed "trained immunity," involving epigenetic reprogramming:
Exposure to microbial components (β-glucan, BCG vaccine, LPS) triggers epigenetic remodeling—histone modifications (H3K4me3, H3K27ac), DNA methylation—enhancing chromatin accessibility at inflammatory gene loci.
Metabolic reprogramming towards glycolysis and increased cholesterol biosynthesis pathways supports enhanced cytokine production (IL-1β, IL-6, TNF-α) upon secondary stimulation.
Clinically relevant in vaccine design, infection resistance (e.g., BCG conferring nonspecific protection), and implicated in pathological conditions (atherosclerosis, chronic inflammation).
Immunosenescence and Aging
Immunosenescence encompasses age-related declines in immune efficacy, driven by intrinsic cellular aging, altered homeostasis, and chronic inflammatory states ("inflammaging"):
Reduced Hematopoietic Stem Cell (HSC) Functionality:
Aging HSCs demonstrate impaired self-renewal, increased myeloid bias, reduced lymphoid progenitor output, diminishing adaptive immunity diversity and resilience.Lymphocyte Repertoire Contraction:
Thymic involution drastically reduces naïve T cell output, narrowing TCR diversity, causing clonal expansion of less-responsive T cells.
B cells exhibit impaired antibody affinity maturation, compromised class-switching, reducing vaccine efficacy.Chronic Low-grade Inflammation ("Inflammaging"):
Persistent innate activation and senescent cells (via senescence-associated secretory phenotype—SASP) secrete IL-6, IL-1β, TNF-α, driving age-associated chronic diseases (cardiovascular disease, neurodegeneration, metabolic syndromes).Innate Immune Dysfunction:
Age-related defects include impaired phagocytosis, reduced cytokine responsiveness, altered antigen presentation (DCs), dysfunctional macrophage polarization, NK cell cytotoxic decline, collectively increasing infection susceptibility and malignancy risk.
Therapeutically addressing immunosenescence—via thymic rejuvenation strategies, senolytics targeting senescent cells, and modulation of metabolic pathways—represents a transformative frontier in aging medicine.
Clinical and Biotechnological Implications
Understanding these advanced immunological topics directly informs biotechnology and therapeutic innovation:
Immune privilege insights guide therapeutic approaches for autoimmune CNS/ocular diseases, transplantation, and infertility treatments.
Harnessing tissue-resident cells (TRMs, microglia) enhances tissue-specific immunotherapy, vaccination strategies, and regenerative medicine.
Trained immunity mechanisms inspire next-generation vaccines with broad protection and novel immunomodulators against chronic inflammation.
Addressing immunosenescence holds promise for improving vaccine responsiveness, treating age-associated diseases, and extending health span.
Specialized immunological research continuously refines our understanding of immune complexity, significantly influencing biotechnology, precision therapeutics, and translational medicine.
Harnessing Immune Cells for Therapeutic Innovation
Decades of research into immune cell biology have culminated in transformative clinical applications. The precise manipulation of immune cell subsets—whether to stimulate, suppress, or redirect their functions—has enabled the development of powerful biotechnological tools across cancer immunotherapy, infectious disease vaccination, and treatment of autoimmune and inflammatory disorders. At the core of these advances is an integrated systems-level understanding of immune cell activation, differentiation, receptor signaling, tissue localization, and regulatory circuitry.
Immune Cell Roles in Disease Contexts
Cancer
Immune surveillance plays a central role in detecting and eliminating malignant cells through mechanisms orchestrated by cytotoxic T lymphocytes (CTLs), natural killer (NK) cells, dendritic cells (DCs), and tumor-associated macrophages (TAMs):
CD8⁺ CTLs detect tumor antigens presented on MHC class I molecules and execute apoptosis via perforin/granzyme release or Fas-FasL interactions.
NK cells contribute to anti-tumor immunity through missing-self recognition (e.g., downregulation of MHC-I on tumors) and ADCC via CD16 (FcγRIII).
Dendritic cells, particularly cDC1, cross-present tumor antigens to naïve CD8⁺ T cells, initiating de novo cytotoxic responses in lymph nodes.
TAMs can adopt either M1-like (pro-inflammatory, anti-tumorigenic) or M2-like (immunosuppressive, tumor-promoting) phenotypes depending on the tumor microenvironment. M2-TAMs suppress T cell activity via IL-10, TGF-β, and arginase-1.
Cancer progression often coincides with immune escape mechanisms including:
Upregulation of checkpoint ligands (e.g., PD-L1, Galectin-9).
Recruitment of Tregs, MDSCs, and M2 macrophages to suppress effector immunity.
Downregulation of antigen presentation machinery (e.g., β2-microglobulin loss).
Infectious Disease
Effective host defense requires a coordinated response between innate and adaptive arms:
Innate immune cells (neutrophils, macrophages, DCs) act within hours of infection, sensing pathogens via PRRs and releasing cytokines (e.g., type I IFNs, IL-1β, IL-12) to shape adaptive responses.
CD4⁺ Th1 cells enhance macrophage function and promote CTL generation through IFN-γ.
CD8⁺ CTLs directly lyse infected cells; their exhaustion (e.g., in chronic LCMV or HIV infection) is marked by elevated inhibitory receptors (PD-1, LAG-3, TIM-3) and altered metabolic profiles.
B cells and plasma cells generate pathogen-specific antibodies that neutralize virions, facilitate opsonization, and fix complement.
Pathogen evasion strategies—such as antigenic variation (HIV, influenza), MHC-I downregulation (HSV, CMV), or immunomodulatory protein secretion (EBV, HCV)—drive the need for immunologically informed vaccine design.
Autoimmunity
Autoimmune pathogenesis reflects a breakdown in self-tolerance at multiple checkpoints:
Autoreactive T cells bypass central or peripheral deletion and recognize self-antigens via aberrant MHC-TCR interactions.
B cells undergo somatic hypermutation and affinity maturation within germinal centers even in the absence of foreign antigens, producing pathogenic autoantibodies (e.g., anti-dsDNA in SLE, anti-CCP in RA).
Tregs are either quantitatively deficient or functionally impaired, failing to restrain effector responses.
Th17 cells produce IL-17A/F and GM-CSF, promoting neutrophil recruitment and tissue damage in diseases such as multiple sclerosis, ankylosing spondylitis, and psoriasis.
Targeted immunomodulation—including depletion of autoreactive B cells (anti-CD20), inhibition of T cell co-stimulation (CTLA4-Ig), or cytokine blockade (anti-IL-17, anti-IL-6R)—relies heavily on immunopathological insights.
Innovative Biotechnological Therapies
1. CAR-T Cell Therapy
Chimeric Antigen Receptor T (CAR-T) cells are autologous T cells genetically engineered to express synthetic receptors comprising:
An extracellular antigen-binding domain (scFv).
A transmembrane domain.
Intracellular signaling domains (e.g., CD3ζ with CD28 or 4-1BB costimulatory motifs).
Mechanism of action:
CARs bypass MHC restriction, enabling T cells to recognize tumor-associated surface antigens (e.g., CD19, BCMA).
Engineered CAR-T cells undergo clonal expansion, cytokine secretion, and direct tumor cell lysis upon antigen engagement.
Clinical challenges and frontiers:
Cytokine Release Syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS).
Resistance via antigen escape (loss of CD19).
Engineering “armored” CAR-T cells that secrete IL-12 or block PD-1 to function within hostile tumor microenvironments.
2. Bispecific Antibodies
Bispecific T-cell engagers (BiTEs) and trispecific formats redirect immune effector cells to tumor cells:
Blinatumomab (anti-CD3 × anti-CD19) bridges T cells and malignant B cells, inducing serial cytolytic synapse formation.
NK cell engagers target CD16 and tumor-associated antigens (e.g., HER2, EGFR), leveraging innate cytotoxicity.
Future formats include conditioned bispecifics that become active only within tumor-specific proteolytic environments, reducing systemic toxicity.
3. mRNA Vaccines
mRNA vaccines use modified nucleoside-containing transcripts (e.g., pseudouridine) encapsulated in lipid nanoparticles (LNPs):
Mechanism: Transfected cells express encoded antigens, which are processed via MHC I/II for T cell priming and antibody production.
Advantages:
Rapid antigen redesign and scalable manufacturing.
Intrinsic adjuvanticity via TLR7/8.
Tailored delivery to dendritic cells or mucosal surfaces.
Applications:
SARS-CoV-2 vaccines (BNT162b2, mRNA-1273).
Neoantigen-targeted cancer vaccines (e.g., personalized melanoma trials).
Therapeutic vaccines for chronic infections (HIV, HBV) and autoimmune modulation (e.g., tolerogenic mRNA constructs encoding autoantigens with immunoregulatory adjuvants).
4. Immune Checkpoint Inhibitors
Checkpoint blockade overcomes T cell exhaustion by targeting inhibitory receptors and restoring effector function:
PD-1/PD-L1 Axis: PD-1 engagement recruits SHP-2 phosphatase, inhibiting proximal TCR signaling and PI3K/Akt pathways; blockade reinvigorates T cell metabolism and cytotoxicity.
CTLA-4: Competes with CD28 for B7 ligands on APCs; blockade promotes T cell priming and reduces Treg-mediated suppression.
Combination therapies:
Dual checkpoint blockade (anti-PD-1 + anti-CTLA-4) shows superior efficacy in melanoma but increases risk of immune-related adverse events.
Emerging checkpoints: LAG-3, TIM-3, TIGIT, VISTA—each with unique intracellular signaling properties and expression patterns in exhausted T cells and tumor-infiltrating lymphocytes (TILs).
Integration of Systems Immunology and Biotechnology
Biotechnological applications increasingly rely on multi-parametric immune profiling, single-cell RNA-seq, spatial transcriptomics, and machine learning to design and optimize therapies:
Personalized Immunotherapy: Leveraging tumor mutanomes and TCR/BCR repertoire analysis to tailor individualized treatments.
Synthetic Biology and Logic Gating: Engineering T cells with AND/OR/NOT logic gates to control activation based on multiple antigen inputs.
Organoid Co-cultures and Humanized Mouse Models: Recapitulate tissue-specific immunity and facilitate translational development.
The translation of immunological insight into clinical biotechnology has fundamentally altered disease management. Immune cells—when properly directed—become precision tools for eliminating tumors, controlling infections, and restoring immune balance. The convergence of immunology, synthetic biology, and systems modeling is rapidly expanding the frontiers of therapeutic innovation, transforming immune cells from biological sentinels into programmable platforms for precision medicine.
Conclusion: The Immune System as a Dynamic and Programmable Network
The immune system is a multi-layered, decentralized biological network composed of diverse, interacting cellular and molecular modules operating across time, space, and context. Rather than functioning as a linear sequence of responses, the immune system exhibits nonlinear dynamics, emergent behavior, self-organization, and stochastic variability. It maintains a delicate balance between immunity and tolerance, defense and repair, destruction and regeneration.
At its core, this system is governed by:
Distributed sensing and signal integration: Via PRRs (e.g., TLRs, NLRs), cytokine receptors, antigen receptors (TCR, BCR), and costimulatory molecules.
Cellular differentiation hierarchies: Rooted in hematopoietic stem cells (HSCs), with branching fate decisions modulated by transcription factor networks (e.g., GATA3, T-bet, FOXP3, BCL6).
Temporal regulation: Responses unfold across discrete time scales—from immediate innate responses (seconds to hours), to adaptive priming (days), to memory maintenance (months to decades).
Tissue compartmentalization and microenvironments: Local stromal, metabolic, and neural inputs define immune cell function, leading to tissue-resident specialization (e.g., TRMs, microglia, Langerhans cells).
This multiscale organization enables robustness and flexibility—yet it also means the immune system cannot be understood or manipulated through reductionist models alone. Immune responses are not simply the outcome of one cell type or cytokine but the result of complex network motifs—such as feedforward loops, feedback inhibition, reciprocal activation, and spatial gating.
Emergent Properties of the Immune System as a Network
Redundancy with specificity: Multiple pathways can converge on similar functional outcomes (e.g., pathogen clearance), but are modulated for context-specific precision (e.g., Th1 vs. Th17 responses against the same microbe in different tissues).
Memory and adaptation: Both adaptive (T and B cell clonal memory) and innate (trained immunity) elements encode prior exposures via epigenetic reprogramming, chromatin accessibility changes, and metabolic rewiring—allowing faster and stronger responses to repeated threats.
Plasticity and state transitions: Immune cells such as macrophages, T helper cells, and ILCs can shift phenotypes in response to environmental cues, exhibiting multi-stability and transdifferentiation potential (e.g., Th17 to Treg under TGF-β influence).
Noise tolerance and stochasticity: Despite variability in gene expression and cell activation thresholds, population-level outcomes (e.g., infection clearance) are reliably achieved through averaging, quorum sensing, and cooperative behaviors.
Resilience and tolerance: Regulatory mechanisms such as Tregs, inhibitory receptors (PD-1, CTLA-4), immunosuppressive cytokines (IL-10, TGF-β), and metabolic brakes (adenosine signaling) prevent overshooting and autoimmunity.
Challenges in Controlling Immune Network Dynamics
Manipulating the immune system therapeutically is complex due to:
Nonlinear dose-response behavior: Cytokine effects are dose-dependent, context-specific, and pleiotropic (e.g., IL-2 can stimulate effector T cells or expand Tregs depending on concentration).
Cellular heterogeneity: Even within defined subsets (e.g., CD8+ T cells), transcriptional and functional heterogeneity exist—necessitating single-cell and spatial resolution for accurate modeling.
Compensatory feedback: Blocking one pathway (e.g., PD-1) often leads to upregulation of parallel suppressive mechanisms (e.g., TIM-3, LAG-3), requiring combinatorial targeting.
Dynamic antigen landscapes: Tumors and pathogens evolve under immune pressure, altering their antigenic makeup and creating escape variants.
Contextual dependence: The same immune molecule (e.g., IL-17) can be protective in mucosal defense and pathogenic in autoimmunity, underscoring the importance of tissue context and timing.
These factors highlight the need for predictive immunological models capable of integrating multi-omic datasets (transcriptomic, proteomic, epigenomic, spatial) and simulating system-wide responses to perturbations.
Outlook: Toward Systems Immunology and Programmable Therapeutics
The future of immunology lies at the intersection of computational modeling, synthetic biology, and AI-driven design. Key directions include:
Systems-level simulation of immune responses: Mechanistic models (e.g., agent-based, differential equation-based, graph-theoretical) are now being used to simulate vaccine responses, immune escape, or tumor-immune dynamics in silico.
Multi-modal immune atlases: Integration of single-cell RNA-seq, ATAC-seq, mass cytometry, and spatial transcriptomics allows detailed reconstruction of immune landscapes across health, disease, and therapeutic response.
AI-guided immunotherapy design:
Predicting optimal neoantigen targets for mRNA vaccines.
Engineering TCRs or CAR constructs with predicted binding affinity and minimal cross-reactivity.
Classifying tumor microenvironments (e.g., inflamed vs. immune-excluded) from histological or transcriptomic data.
Synthetic immune circuits: Using synthetic biology, immune cells can now be programmed with Boolean logic gates (e.g., AND, OR, NOT) to respond only to specific combinations of inputs (e.g., dual tumor antigens, hypoxia + checkpoint ligand), minimizing off-target effects.
This convergence of data-driven modeling and programmable interventions is giving rise to “immune operating systems”—therapies designed not just to activate the immune system, but to rewire its logic in a controlled and predictable manner.
Final Perspective
The immune system is no longer viewed as a chaotic ensemble of reactive cells—it is increasingly understood as a programmable, adaptive network with measurable inputs, definable states, and engineerable outputs. As we develop the tools to map and model this network with precision, immunology is becoming the central operating system of biomedicine.
Whether through systems-level vaccination, CAR-engineered cell therapies, immune checkpoint integration, or digital immune modeling, the ability to program immune responses with precision will define the next generation of biotechnology.